According to UCLA Health, roughly one in three women will experience a pelvic floor disorder (PFD) in her lifetime. From research conducted by the Royal College of Obstetricians and Gynecologists (RCOG), only 53% will ever seek out some type of treatment.
Over the years, physical therapy has become one of the best first steps for those seeking treatment for pelvic floor disorder. While there might be different factors causing pelvic floor disorder, the approach of our PFD therapists at Advance Rehabilitation Physical Therapy is centered around eliminating or managing pelvic pain/problems while restoring their quality of life.
Below are 4 common pelvic floor conditions that can be treated with physical therapy.
- Pelvic floor pain or dysfunction
- Pelvic organ prolapse (POP)
- Postpartum recovery and or pain
- Urinary incontinence
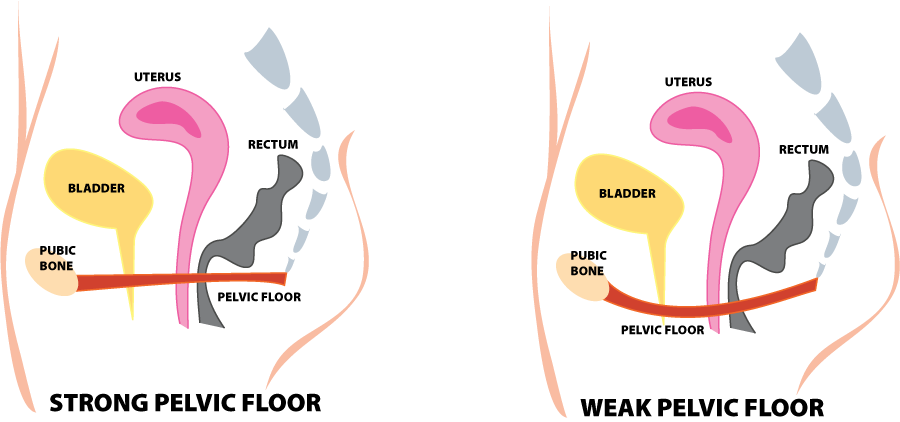
Pelvic Floor Pain or Dysfunction
Pelvic pain can occur for many reasons. One typical cause is what is called a hypertonus dysfunction or an unusual tightening of the pelvic floor muscles. This is common after a long delivery and scar tissue formation from a healing episiotomy.
Pelvic floor pain/dysfunction can also occur from sexual abuse or when the muscles tighten to prevent the “falling out” sensation that occurs with the prolapse of the internal organs. The primary symptom is pain, which can occur in the back, perivaginal area, lower abdomen, or thighs.
How physical therapy can help pelvic pain patients:
Physical therapy can help to eliminate or manage pelvic pain while restoring the quality of life. This is possible through a comprehensive approach to evaluating and treating the pelvic floor. According to Kaitlyn Boone, PT, DPT, Women’s Health Specialist with Advance Rehabilitation at East Cobb, “There are a variety of techniques and tools focused on relaxation of the pelvic floor muscles that can be utilized for pelvic pain including manual therapy techniques, stretching, breathing techniques, and education. The use of home devices such as dilators or pelvic wands can be incorporated into a patient’s treatment plan to improve one’s pain and function.”
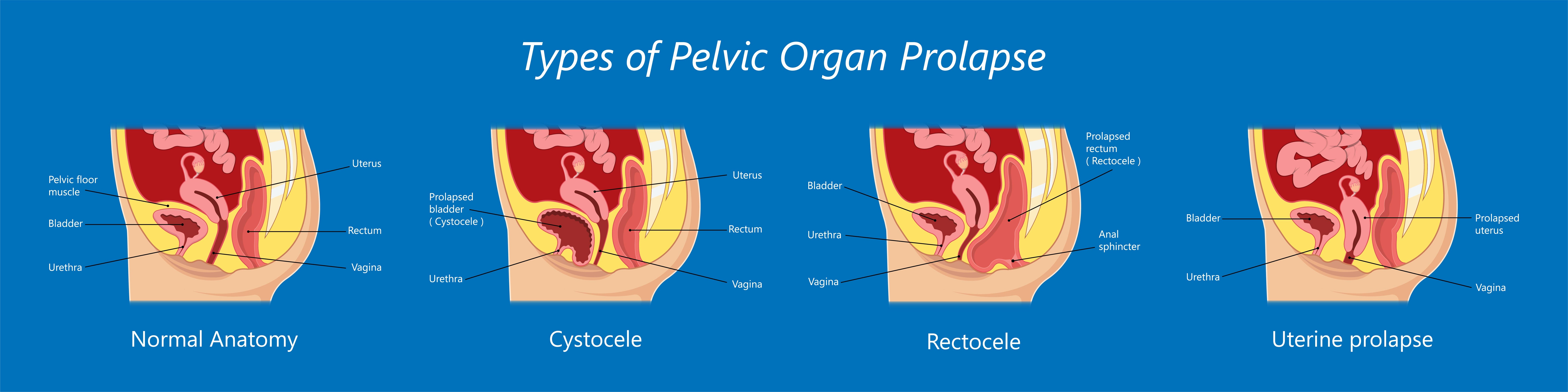
Pelvic Organ Prolapse
According to the International Urogynecology Association (IUGA) and the International Continence Society (ICS), pelvic organ prolapse is defined as the descent of one or more of the anterior vaginal wall, the posterior vaginal wall, the uterus (cervix) or the apex of the vagina (vaginal vault or cuff after hysterectomy). POP can be caused by a variety of circumstances, including vaginal childbirth, increased age and/or BMI, increased abdominal pressure, and connective tissue disorder. While many women can be asymptomatic, some of the symptoms of pelvic organ prolapse (POP) include:
- The sensation of pressure or heaviness in the vagina
- A feeling of bulging or something coming out of the vagina
- Urinary symptoms: incontinence, position change or manual reduction of prolapse needed to initiate or complete voiding, weak or prolonged stream, incomplete emptying, obstructed voiding symptoms
- Bowel symptoms: incontinence, feeling of incomplete emptying, straining, digital evacuation, splinting of vagina or perineum to aid emptying
- Sexual symptoms: decreased lubrication, sensation, arousal, or dyspareunia
How physical therapy can help pelvic organ prolapse patients:
- Pelvic floor muscle training (recommended as the first line of treatment in stages 1-2 of pelvic organ prolapse)
- Strength and endurance training of underactive pelvic floor
- Stretching and relaxation of an overactive pelvic floor
- Lifestyle modification to reduce the effect of increased abdominal pressure on the pelvic organ support system
In addition to physical therapy, other treatments for POP may include pharmacological treatment, the use of mechanical devices, and surgical intervention.
Post Partum Recovery and/or Pain
Birthing a baby is a joyful and yet very traumatic experience. Regardless of the method of delivery, whether VBAC or Cesarean Section, each birth comes with its own potential postpartum problems. From urinary incontinence to pelvic pain, there are just some things after childbirth that are not glamorous and can be embarrassing to discuss.
While some issues will resolve over time, there may be treatments that can help. Pelvic health physical therapy can address diastasis recti (a tear in the abdominal wall), urinary incontinence, low back/ pelvic girdle/hip pain, pain with intercourse, or scar pain, to name a few postpartum unpleasantries that may benefit from physical therapy.
Potential postpartum problems that can be helped with physical therapy:
- Urinary incontinence
- Pain with intercourse
- Pelvic floor pain
- Scar pain
- Diastasis recti
- Pelvic organ prolapse
- Difficulty returning to exercise
If you find yourself six weeks postpartum and still suffering, please discuss this with your OB-GYN and decide if a referral to physical therapy may help.
Urinary Incontinence
Urinary incontinence can be embarrassing, but it doesn’t have to be part of your life. Do you have to change pads every couple of hours? Is there a worry about going out because you need to know where the closest bathroom is? Do you always carry a change of clothes with you? Do you not travel or exercise because of fear of leakage? Don’t live in fear of urinary leakage.
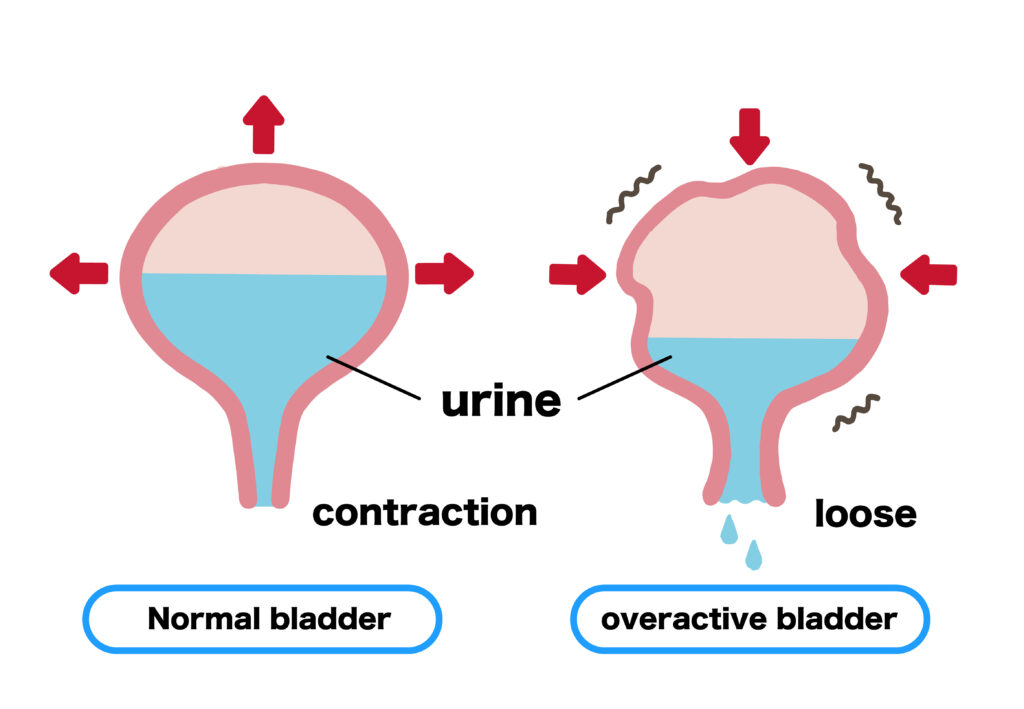
Symptoms of Urinary Incontinence Include:
- Involuntary loss of urine
- Increased daytime/ nighttime frequency
- Urgency
- Post voiding retention
- Straining to avoid dribble
- Efforts like coughing or other activities can cause leakage
How physical therapy can help urinary incontinence patients:
- Behavioral interventions (urge suppression techniques, dietary modifications, appropriate fluid intake, weight loss, habit training)
- Pelvic muscle re-training (for overactive) as well as underactive pelvic floor
- Bladder training (bladder diary or scheduled voiding)
- Neuromuscular re-education (NMES) and biofeedback devices
What to expect during a women’s health physical therapy session:
Each person will be individually evaluated and treated in a quiet, private, safe space. If the patient is comfortable, the initial evaluation may include an internal exam to assess the patient’s musculature and symptoms properly. According to Katherine Frierson, PT, DPT, and Women’s Health Specialist, “A thorough examination will be performed, including a detailed history and discussion of the patient’s concerns and goals for physical therapy. Women of all ages and backgrounds are encouraged to participate.”
- Musculoskeletal Assessment: An evaluation to identify causes of poor postural alignment, strength, flexibility, and movement patterns that cause orthopedic pain.
- Soft Tissue Mobilization: To release adhesional restrictions.
- Observation and palpation of the pelvic floor to the patient’s comfort level
- Stretching and strengthening techniques
- Relaxation techniques
- Soft tissue and joint mobilization
- Modalities: Interferential electrical stimulation, ultrasound, heat or cold therapy.
- Biofeedback: Provides measurable assessment of the pelvic floor muscles’ ability to contract and relax in function.
- Behavior modification
- Educational instruction: Home exercise programs and information concerning diet, sleep, work and rest positions, and self-management of symptoms.
Seeking Treatment:
If you are a woman suffering from a pelvic floor disorder (PFD), Advance Rehabilitation Physical Therapy is here to help. Our pelvic floor-trained therapists are ready to provide a customized treatment plan that addresses your symptoms and works toward your established goals. If you need to schedule an appointment with any of our Women’s Health Specialists, please contact one of our clinics listed below or click here to schedule an appointment online.
ADVANCE REHAB EAST COBB / MARIETTA
1000 Johnson Ferry Road, Suite A-115
Marietta, GA 30068
Phone: 404.367.2085
Fax: 770.579.7060
ADVANCE REHAB / COLUMBUS
3709 Gentian Blvd., Suite 12
Columbus, GA 31907
Phone: 706-887-5665
Fax: 706-887-5672
ADVANCE REHAB / FOLKSTON
215 First Street
Folkston, GA 31537
T: 912.496.7842
F: 912.496.4617
KINGSLAND / ST MARYS
100 A Lindsey Lane
St. Marys, GA 31558
T: 912.729.1333
F: 912.729.5259